POC creatinine, urea and eGFR* help accelerate ED workflows[1]
Fast recognition of Acute Kidney Injury (AKI) reduces patient mortality and complications [2]
Strengthen ED care with POC kidney function testing
Acute Kidney Injury (AKI) is seen in 13-18% of all people admitted to the hospital, and early intervention to reduce mortality and complications is vital [2].
Accelerate clinical decision-making and reduce length of stay for patients requiring contrast-enhanced CT-scan, all with one analyser and from one sample at the POC [3].
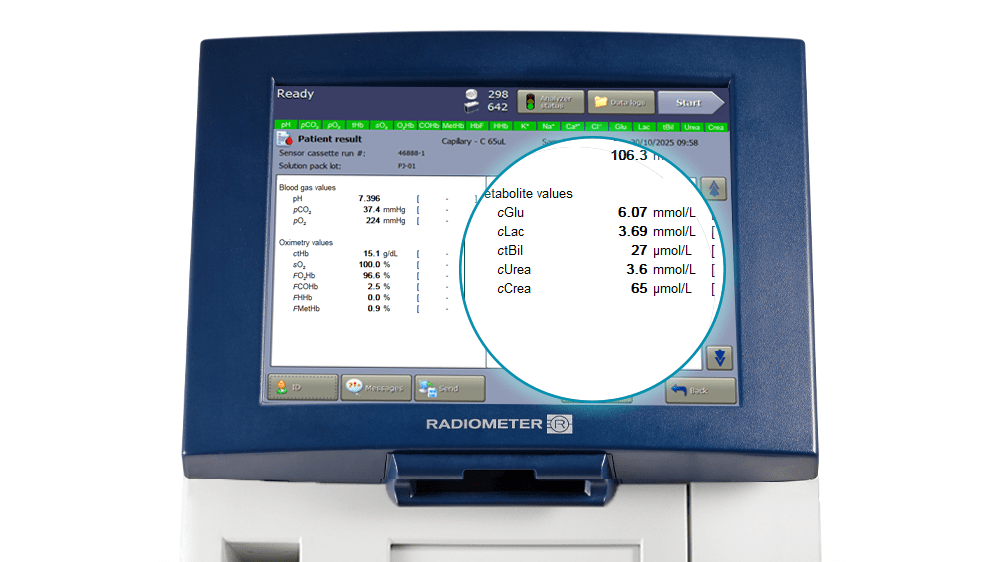
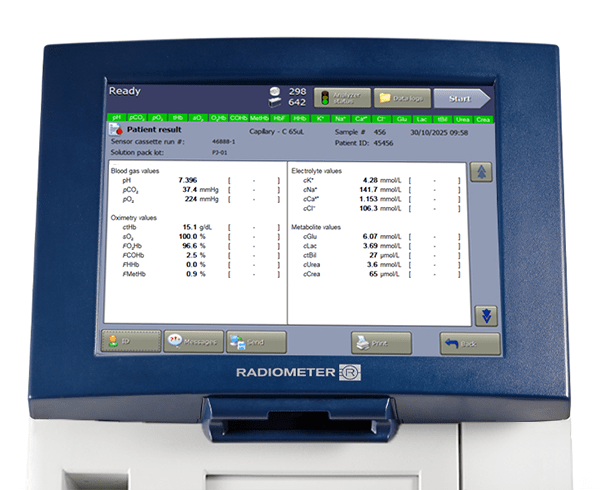
With the ABL90 FLEX PLUS blood gas analyser, you can add creatinine, urea, and eGFR to your emergency panel using only 65 μL of whole blood and receive 19 results within 35 seconds.
19 parameters
The ABL90 FLEX PLUS blood gas analyser measures up to 19 parameters
Renal markers: Creatinine, urea, and eGFR
Parameters measured
Potential of hydrogen
The degree of acidity or alkalinity of any liquid (including blood) is a function of its hydrogen ion concentration [H+], and pH is simply a way of expressing hydrogen ion activity. The relationship between pH and hydrogen ion concentration is described thus:
pH = -log aH+
where aH+ is hydrogen ion activity.
Low pH is associated with acidosis and high pH with alkalosis [1,2].
- CLSI. Blood gas and pH analysis and related measurements; Approved Guidelines. CLSI document CA46-A2, 29, 8. Clinical and Laboratory Standards Institute, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2009
- Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook
Partial pressure of carbon dioxide
Carbon dioxide (CO2) is an acidic gas; the amount of CO2 in blood is largely controlled by the rate and depth of breathing or ventilation. pCO2 is the partial pressure of CO2 in blood. It is a measure of the pressure exerted by that small portion (~5 %) of total CO2 that remains in the gaseous state, dissolved in the blood plasma. pCO2 is the respiratory component of acid-base balance and reflects the adequacy of pulmonary ventilation. The severity of ventilator failure as well as the chronicity can be judged by the accompanying changes in acid-base status [1,2].
- Higgins C. Parameters that reflect the carbon dioxide content of blood. www.acutecaretesting.org Oct 2008.
- Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014
Partial pressure of oxygen
The amount of oxygen in blood is controlled by many variables, e.g. ventilation/perfusion. pO2 is the partial pressure of oxygen in a gas phase in equilibrium with the blood. pO2 only reflects a small fraction (1 – 2 %) of total oxygen in blood that is dissolved in blood plasma [1]. The remaining 98 – 99 % of oxygen present in blood is bound to the hemoglobin in the erythrocytes. pO2 primarily reflects the oxygen uptake in the lungs. [2]
1. Wettstein R, Wilkins R. Interpretation of blood gases. In: Clinical assessment in respiratory care, 6th ed. St. Louis: Mosby, 2010.
2. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Glucose
Glucose, the most abundant carbohydrate in human metabolism, serves as the major intracellular energy source (see lactate). Glucose is derived principally from dietary carbohydrate, but it is also produced – primarily in the liver and kidneys – via the anabolic process of gluconeogenesis, and from the breakdown of glycogen (glycogenolysis). This endogenously produced glucose helps keep blood glucose concentration within normal limits, when dietary-derived glucose is not available, e.g. between meals or during periods of starvation. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Lactate, the anion that results from dissociation of lactic acid, is an intracellular metabolite of glucose. It is produced by skeletal muscle cells, red blood cells (erythrocytes), the brain, and other tissues during anaerobic energy production (glycolysis). Lactate is formed in the intracellular fluid from pyruvate; the reaction is catalyzed by the enzyme lactate dehydrogenase (LDH) [1,2].
1. Robergs RA, Ghiasvand F, Parker D. Biochemistry of exercise-induced metabolic acidosis. Am J Physiol Regul Integr Comp Physiol 2004; 287: R502-16.
2. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Creatinine
Creatinine is an endogenous waste product of muscle metabolism, derived from creatine, a molecule of major importance for energy production within muscle cells. Creatinine is removed from the body in urine and its concentration in blood reflects glomerular filtration and thereby kidney function. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Urea
Urea (molecular formula CO(NH2)2) is the principal nitrogenous waste product of protein catabolism, which is eliminated from the body in urine. It is the most abundant organic component of urine. Urea is transported in blood from the liver to the kidneys, where it is filtered from the blood and excreted in the urine. Renal failure is associated with the reduced excretion of urea in urine, and a consequent rise in blood (plasma/serum) urea concentration. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Calsium
The calcium ion (Ca2+) is one of the most prevalent cations in the body, where approximately 1 % is present in the extracellular fluid of blood. Ca2+ plays a vital role for bone mineralization and many cellular processes, e.g. contractility of the heart and the skeletal musculature, neuromuscular transmission, hormone secretion and action in various enzymatic reactions such as, e.g. blood coagulation. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Chloride
Chloride (Cl-) is the major anion in the extracellular fluid and one of the most important anions in blood. The main function of Cl- is to maintain osmotic pressure, fluid balance, muscular activity, ionic neutrality in plasma, and help elucidate the cause of acid-base disturbances. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Potassium
Potassium (K+) is the major cation in the intracellular fluid, where it has a 25 - 37-fold higher concentration (∼150 mmol/L in tissue cells, ∼105 mmol/L in erythrocytes) than in the extracellular fluid (∼4 mmol/L) [1, 2]. K+ has several vital functions in the body, e.g. regulation of neuromuscular excitability, regulation of heart rhythm, regulation of intracellular and extracellular volume and acid-base status. [3]
1. Burtis CA, Ashwood ER, Bruns DE. Tietz textbook of clinical chemistry and molecular diagnostics. 5th ed. St. Louis: Saunders Elsevier, 2012.
2. Engquist A. Fluids/Electrolytes/Nutrition. 1st ed. Copenhagen: Munksgaard, 1985.
3. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Sodium
Sodium (Na+) is the dominant cation in the extracellular fluid, where it has a 14-fold higher concentration (∼140 mmol/L) than in the intracellular fluid (∼10 mmol/L). Na+ is a major contributor of the osmolality of the extracellular fluid and its main function is largely in controlling and regulating water balance, and maintaining blood pressure. Na+ is also important for transmitting nerve impulses and activating muscle concretion. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Carboxyhemoglobin
FCOHb is the fraction of total hemoglobin (ctHb) which is present as carboxyhemoglobin (COHb). By convention the fraction is expressed as a percentage (%).
In the range of 0 – 60 % COHb in arterial (COHb(a)) and venous blood (COHb(v)) is similar, i.e. either venous or arterial blood may be analyzed [1]. In most medical texts FCOHb(a) is referred to as simply COHb. [2]
1. Lopez DM, Weingarten-Arams JS, Singer LP, Conway EE Jr. Relationship between arterial, mixed venous and internal jugular carboxyhemoglobin concentrations at low, medium and high concentrations in a piglet model of carbon monoxide toxicity. Crit Care Med 2000; 28: 1998-2001.
2. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Bilirubin
Bilirubin is the yellow breakdown product of the degradation of the heme group of hemoglobin. It is transported in blood from its site of production – the reticuloendothelial system – to the liver, where it is biotransformed before excretion in bile. Jaundice, the pathological yellow discoloration of skin, is due to abnormal accumulation of bilirubin in the tissues, and is always associated with elevated blood concentration of bilirubin (hyperbilirubinemia). [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Total hemoglobin
The concentration of total hemoglobin (ctHb) in blood includes oxyhemoglobin (cO2Hb), deoxyhemoglobin (cHHb), as well as the dysfunctional hemoglobin species that are incapable of binding oxygen:
carboxyhemoglobin (cCOHb) (see COHb), methemoglobin (cMetHb) (see MetHb) and sulfhemoglobin (cSulfHb).
Thus:
ctHb = cO2Hb + cHHb + cCOHb + cMetHb + cSulfHb
The rare sulfHb is not included in the reported c tHb in most oximeters. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Fraction of fetal hemoglobin
FHbF in total hemoglobin in blood. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Fraction of deoxyhemoglobin
FHHb in total hemoglobin in blood. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Metahemoglobina
FMetHb is the fraction of total hemoglobin (ctHb) that is present as methemoglobin (MetHb). By convention the fraction is expressed as a percentage (%) [1]. In most medical text boxes MetHb(a) is referred to as simply methemoglobin (MetHb). [2]
1. CLSI. Blood gas and pH analysis and related measurements; Approved Guidelines. CLSI document CA46-A2, 29, 8. Clinical and Laboratory Standards Institute, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2009.
2. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
Oxygen saturation
Oxygen saturation (sO2) is the ratio of oxyhemoglobin concentration to concentration of functional hemoglobin (i.e. oxyhemoglobin (O2Hb) and deoxyhemoglobin (HHb) capable of carrying oxygen [1].
The sO2 reflects utilization of the currently available oxygen transport capacity. In arterial blood 98 – 99 % of oxygen is transported in erythrocytes bound to hemoglobin. The remaining 1–2 % of the oxygen transported in blood is dissolved in the blood plasma – this is the portion reported as partial pressure of oxygen (pO2) [2,3].
1. CLSI. Blood gas and pH analysis and related measurements; Approved Guidelines. CLSI document CA46-A2, 29, 8. Clinical and Laboratory Standards Institute, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2009.
2. Higgins C. Parameters that reflect the carbon dioxide content of blood. www.acutecaretesting.org Oct 2008.
3. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on /en/knowledge-center/handbooks/acute-care-testing-handbook.
Fraction of oxyhemoglobin
FO2Hb in total hemoglobin in blood. [1]
1. Acute care testing handbook. Radiometer Medical ApS, 2700 Brønshøj, Denmark, 2014. As accessed on https://www.radiometer.com/en/knowledge-center/handbooks/acute-care-testing-handbook.
*eGFR is calculated
Faster diagnosis and treatment with creatinine, urea and eGFR results for patients requiring contrast enhanced CT scan [3]
- ✓Earlier AKI risk identification supports faster clinical escalation [4].
- ✓Contrast imaging suitability is decided on the spot, using real-time estimated GFR [2].
- ✓Nephrotoxic drugs are prescribed with confidence, guided by known renal function [3,5].
- ✓Dehydration is confirmed quickly, using urea to support clinical judgement [6].
After two minutes we can already give the patient a contrast medium during the CT scan, and we know the creatinine levels so we can better assess the risk of possible complications.
- Axel Plessmann, ED Director, DRK Hospital Group, Germany (ABL90 FLEX PLUS user)
Click here to renew consent
Learn how the ABL90 FLEX PLUS blood gas analyser with creatinine, urea, and eGFR results empower you to act with speed and confidence
POC creatinine improves ED workflow
Studies suggest that POC creatinine, urea can help improve ED workflows.
Minimal interference on creatinine
Creatinine measurement on the ABL90 FLEX PLUS blood gas analyser shows minimal interference.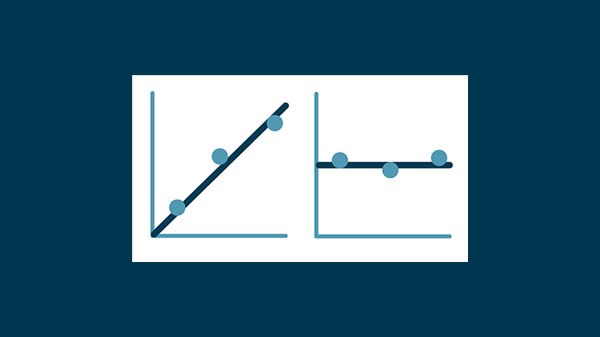
Excellent performance vs established lab methods
Creatinine measurement on the ABL90 FLEX PLUS blood gas analyser shows excellent agreement vs 4 lab methods.
ABL90 FLEX PLUS blood gas analyser
- Fast analysis
- Reliable results
- Easy to use and maintain
ABL90 FLEX PLUS blood gas analyser
Emergency department point-of-care-testing solutions
Scientific articles on acutecaretesting.org
FAQ: Kidney function testing at the point of care (creatinine, urea & eGFR)
Can the ABL90 FLEX PLUS blood gas analyser really provide lab quality results in 35 seconds?
Yes, it can. Scientific research evaluation confirms that Radiometer ABL90 FLEX PLUS creatinine enzymatic assay is at least as suitable as a conventional clinical chemistry enzymatic technique for routine and urgent diagnosis of kidney diseases [7].
Does adding creatinine and urea parameters to the blood gas analyser enable faster diagnostic decisions in the emergency department?
In the ED, the initial diagnostic decisions are based on a panel of different parameters, including crea/urea. Because creatinine and urea are used for certain specific risk stratifications and differential diagnoses, the readily availability of these parameters at POC will allow faster decisions than if the test results were provided from a central laboratory.
How can the ABL90 FLEX PLUS help improve patient flow in the ED by offering more parameters?
A study by Jimenez found that a strategy based on POCT improves patient flow in the ED and was more effective and less expensive than standard care. In the study, emergency patients were divided into two different groups, interventional arm (analyses performed on POCT analyzers in the Emergency Department: Blood gas, Basic Metabolite Panel, hematology, urine, coagulation) or control arm (central laboratory). There was a significant reduction in the outcome of LOS of 88.50 min, TDD of 89.00 min and LTAT of 67.11 min. No increase in readmission was found. There was also a significant reduction in the associated cost using the POCT approach compared with the strategy used in usual care. [8]
In which situations is point of care analysis of creatinine, urea, and eGFR most useful in the ED?
There are several uses. Recognising AKI, confirming contrast imaging eligibility, investigation renal Clearance, and assessing renal status before administering nephrotoxic drugs are among the most common. These ensure fast, informed decisions about patient care, as well as improved efficiency in the ED. Other uses include:
- Helping to identify if the cause of AKI is pre-renal, intrinsic renal, or post-renal [9, 10, 11].
- Aiding in identifying undiagnosed chronic kidney disease (CKD) [12].
- Evaluating patient dehydration [13].
- Assessing pneumonia severity. (e.g., CURB-65) [14,15].
- Helps assess upper gastrointestinal bleeds. (e.g., Glasgow-Blatchford Score) [16,17,18].
- Supporting acute pancreatitis assessment. (creatinine associated with severity) [19,20].
- Aiding in recognising sepsis. (For the renal component) [21,22,23].
Which other parameters are measured on the ABL90 FLEX PLUS blood gas analyser?
Rapid 19 parameters – including blood gas, metabolites, electrolytes, hemoglobin, and renal. These are measured on the ABL90 FLEX PLUS blood gas analyser from 1 sample, giving all answers in 35 seconds from 65 μl of blood. The full list of measured parameters is:
Blood gas: pH, pCO2, pO2
Metabolites: cLac, cGlu,
Electrolytes: cNa+, cK+, cCa2+, cCl-
Hemoglobin: FCOHb, ctHb, FHbF, FHHB, FMetHb, sO2, FO2Hb, ctBil
Renal: cCrea, cUrea/, eGFR(calc)
References
2. NICE National Institute for Health and Care Excellence. Acute kidney injury: prevention, detection and management. NICE guideline 2019. Overview | Acute kidney injury: prevention, detection and management | Guidance | NICE. Accessed Nov 2025 Polavarapu
3. European Society of Urogenital Radiology. ESUR Guidelines on Contrast Agents version 10.0. ESUR GUIDELINES ON CONTRAST AGENTS | esur.org. Accessed Nov. 2025
4. Polavarapu M, Groner K, Craig BA, Eilman V, Costinas S. Using Point-of-Care Creatinine Testing as a Vehicle to Expedite Patient Care. Annals of Emergency Medicine 2020; 76, 4S.
5. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney inter., Suppl. 2012; 2: 1–138.
6. Gianfranco Sanson, Ilaria Marzinotto, Daniela De Matteis, Giuliano Boscutti, Rocco Barazzoni, Michela Zanett; Impaired hydration status in acutely admitted older patients: prevalence and impact on mortality. Published by Oxford University Press on behalf of the British Geriatrics Society. Age and Ageing 2021; 50: 1151–1158 https://doi.org/10.1093/ageing/afaa264 Published electronically 16 December 2020
7. Salvagno, G. L., Pucci, M., Demonte, D., Gelati, M., & Lippi, G. (2019). Analytical evaluation of Radiometer ABL90 FLEX PLUS enzymatic creatinine assay. Journal of Laboratory and Precision Medicine, 4, 26. https://doi.org/10.21037/jlpm.2019.07.01
8. Jimenez-Barragan, M., Rodriguez-Oliva, M., et al. Emergency severity level-3 patient flow based on point-of-care testing improves patient outcomes. 2021; 144-151. Clin Chim Acta. https://doi.org/10.1016/j.cca.2021.09.011
9. James Taylor; Renal system 3: categorizing, assessing and managing acute kidney injury; Nursing Times [online] April 2003 / vol 119 issue 4
10. Michael G Mercado MD, Dustin K Smith DO and Esther L Guard DO; Acute Kidney Injury: Diagnosis and Management; American Family Physician; December 1, 2009, vol 100, number 11
11. Chris Nickson; Urea-Creatinine Ratio, Life in the Fastlane, July 28 2024; https://litfl.com/urea-creatinine-ratio/
12. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105(4S):S117-S314. doi:10.1016/j.kint.2023.10.018
13. Trainor JL, Glaser NS, Tzimenatos L, Stoner MJ, Brown KM, McManemy JK, Schunk JE, Quayle KS, Nigrovic LE, Rewers A, Myers SR, Bennett JE, Kwok MY, Olsen CS, Casper TC, Ghetti S, Kuppermann N; Pediatric Emergency Care Applied Research Network (PECARN) FLUID Study Group. Clinical and Laboratory Predictors of Dehydration Severity in Children With Diabetic Ketoacidosis. Ann Emerg Med. 2023 Aug;82(2):167-178. doi: 10.1016/j.annemergmed.2023.01.001. Epub 2023 Apr 5. PMID: 37024382; PMCID: PMC10523885.
14. Lim, W. S., Van der Eerden, M. M., Laing, R., Boersma, W. G., Karalus, N., Town, G. I., ... & Macfarlane, J. (2003). Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax, 58(5), 377-382.
15. National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. London: ICE; 2023. CG191. https://www.nice.org.uk/guidance/cg191 (accessed 18 Mar 2025)
16. Kumar NL, Claggett BL, Cohen AJ, Nayor J, Saltzman JR. Association between an increase in blood urea nitrogen at 24 hours and worse outcomes in acute nonvariceal upper GI bleeding. Gastrointest Endosc. 2017 Dec;86(6):1022-1027.e1. doi: 10.1016/j.gie.2017.03.1533. Epub 2017 Apr 2. PMID: 28377105.
17. Richards, Robert J. M.D.; Donica, Mary Beth M.D.; Grayer, David M.D.. Can the Blood Urea Nitrogen/Creatinine Ratio Distinguish Upper From Lower Gastrointestinal Bleeding?. Journal of Clinical Gastroenterology 12(5):p 500-504, October 1990
18. Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000 Oct 14;356(9238):1318-21. doi: 10.1016/S0140-6736(00)02816-6. PMID: 11073021
19. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2012;62(1):102-111. doi:10.1136/gutjnl-2012-302779
20. Mederos MA, Reber HA, Girgis MD. Acute Pancreatitis: A Review. JAMA. 2021 Jan 26;325(4):382-390. doi: 10.1001/jama.2020.20317. Erratum in: JAMA. 2021 Jun 15;325(23):2405. doi: 10.1001/jama.2021.5789. PMID: 33496779.
21. Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. Sepsis-Associated Acute Kidney Injury. Crit Care Clin. 2021 Apr;37(2):279-301. doi: 10.1016/j.ccc.2020.11.010. Epub 2021 Feb 13. PMID: 33752856; PMCID: PMC7995616.
22. Gounden V, Bhatt H, Jialal I. Renal Function Tests. [Updated 2024 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507821/
23. National Institute for Health and Care Excellence . Sepsis: recognition, diagnosis and early management. London: ICE; 2025. NG51. https://www.nice.org.uk/guidance/ng51 (accessed 18 Mar 2025)
Cookies are used on this website
Use of cookiesPlease enter a valid email
We will be sending an e-mail invitation to you shortly to sign in using Microsoft Azure AD.
It seems that your e-mail is not registered with us
Please click "Get started" in the e-mail to complete the registration process
Radiometer is using Microsoft AZURE Active Directory to authenticate users
Radiometer uses Azure AD to provide our customers and partners secure access to documents, resources, and other services on our customer portal.
If your organization is already using Azure AD you can use the same credentials to access Radiometer's customer portal.
Key benefits
- Allow the use of existing Active Directory credentials
- Single-sign on experience
- Use same credentials to access future services
Request access
You will receive an invitation to access our services via e-mail when your request has been approved.
When you accept the invitation, and your organization is already using AZURE AD, you can use the same credentials to access Radiometer's customer portal. Otherwise, a one-time password will be sent via e-mail to sign in.